What is the "allowed" amount on my dental insurance policy?
When visiting an In-Network provider, the "allowed" amount is the maximum amount the policy will pay for a covered service. Your policy will then pay a percentage of the allowable amount.
In-Network
Joanne has had her policy for 13 months and has selected an in-network dentist for her dental work. Her dental provider agreed to a discounted rate for services as an in-network dentist, which means she paid $647.40 for her dental treatment (including $100 deductible).
| Service |
Billed** |
In-Network Discount |
Allowed*** |
Paid % |
Plan Pays |
Deductible |
Patient Pays* |
| Filling |
$250.00 |
$152.00 |
$98.00 |
70% |
$68.60 |
$0.00 |
$29.40 |
| Crown* |
$1,200.00 |
$487.00 |
$713.00 |
60% |
$367.80 |
$100.00 |
$345.20 |
| Root Canal |
$800.00 |
$118.00 |
$682.00 |
60% |
$409.20 |
$0.00 |
$272.80 |
| TOTAL |
$2,250.00 |
$757.00 |
$1,493.00 |
|
$845.60 |
$100.00 |
$647.40 |
*Including $100 deductible as outlined in your policy.
**Billed amounts are based on actual claims and will vary by dentist.
*** The In-Network Allowed amount is based on the Maximum Care PPO CI-5 fee schedule and will vary by area.
Can I see an out-of-network dentist?
Yes. However, dentists who are not in-network may bill you their normal fee for procedures. Your plan provides benefits using amounts that we have set as the "maximum allowed amount" for each service in your geographic area. When we set the "maximum allowed amount," we may consider other factors, including the prevailing charges in your area. The "maximum allowed amount" does not suggest your dentist's fees are not reasonable and proper.
Your dentist may bill you for the difference between his or her normal fee and our "maximum allowed amount." This amount is not covered, and you must pay it.
Out-of-Network
Joanne has had her policy for 13 months and has selected an out-of-network dentist for her dental work. She paid $1,404.40 (including $100 deductible) for her dental treatment.
| Service |
Billed** |
Allowed*** |
Paid % |
Plan Pays |
Deductible |
Patient Pays* |
| Filling |
$250.00 |
$98.00 |
70% |
$68.60 |
$0.00 |
$181.40 |
| Crown* |
$1,200.00 |
$713.00 |
60% |
$367.80 |
$100.00 |
$832.20 |
| Root Canal |
$800.00 |
$682.00 |
60% |
$409.20 |
$0.00 |
$390.80 |
| TOTAL |
$2,250.00 |
$1,493.00 |
|
$845.60 |
$100.00 |
$1,404.40 |
*Including $100 deductible as outlined in your policy.
**Billed amounts are based on actual claims and will vary by dentist.
*** The Out-of-Network Allowed amount is based on the Maximum Care PPO CI-5 fee schedule and will vary by area.
When can I start using my policy?
You can start using your policy as soon as your policy is effective.
Why does it cost less to see an in-network provider than an out-of-network provider?
In-network providers have agreed to offer services at a negotiated discounted rate. If you visit an in-network provider, you "may" pay less out of pocket.
How do I find an in-network provider?
Visit the Provider Search page.
Who do I reach out to if my provider isnt accepting the plan?
Contact Customer Care at 1-833-468-4340
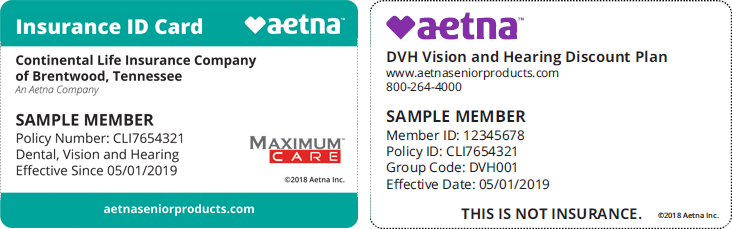
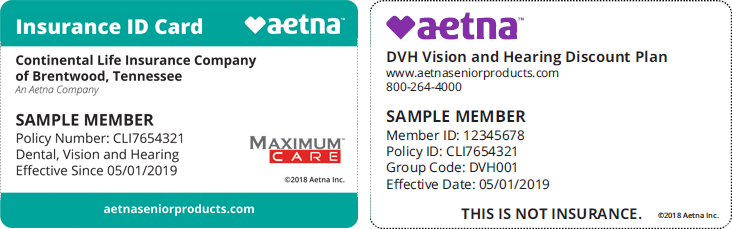
How can I save additional money on vision and hearing care?
Your policy includes value-added discounts on eye care services, eyewear, LASIK vision correction surgery and hearing aids. By selecting an in-network vision or hearing care provider, you will pay a discounted rate. With these discounts, you can reduce your out-of-pocket expenses. When you file a claim, the discounted rate will be reflected, which means you'll have more left of your benefit maximum to use for other services. You can submit a claim for reimbursement for your vision and hearing care here.
How do I file a claim for my vision and hearing benefit?
For Vision and Hearing claims, please use the Vision and Hearing Claim Form. Click Here for more claims information.
My dentist didn't file my claim?
Dental claims should be submitted by your provider.
If your provider did not submit your claim, you can submit your claim here.
What is the status of my claim?
Claim status can be found under "My Health Plan claim status" in the "Claims Portal". You can register for the claims portal here: https://carmwp.skygenusasystems.com/MWP/Landing
Once registered, you can log in to the member portal here: https://carmwp.skygenusasystems.com/MWP/Landing
How do I appeal a claim?
Appeals must be submitted in writing via email to [email protected].
What is my member ID number and where can I locate it?
Your member ID number is a unique identifier that helps protect your identity and can be found:
- On your secure Member Dashboard
- On your Dental ID card
- By calling our Customer Care Team
What does Careington handle and what does Aetna handle?
Careington handles the following:
- Provider search
- Details about your claims
- Benefit breakdowns
- Fulfillment requests
Meanwhile, Aetna handles the following:
- Billing/payment updates
- Policy changes
- Agents
- Member Portal issues
Contact Customer Care at 1-833-468-4340 or login in to your member portal

What is the "allowed" amount on my dental insurance policy?
When visiting an In-Network provider, the "allowed" amount is the maximum amount the policy will pay for a covered service. Your policy will then pay a percentage of the allowable amount.
In-Network
Joanne has had her policy for 13 months and has selected an in-network dentist for her dental work. Her dental provider agreed to a discounted rate for services as an in-network dentist, which means she paid $767.10 for her dental treatment (including $100 deductible).
| Service |
Billed** |
In-Network Discount |
Allowed*** |
Paid % |
Plan Pays |
Deductible |
Patient Pays* |
| Filling |
$250.00 |
$152.00 |
$98.00 |
80% |
$78.40 |
$0.00 |
$19.60 |
| Crown* |
$1,200.00 |
$487.00 |
$713.00 |
50% |
$306.50 |
$100.00 |
$406.50 |
| Root Canal |
$800.00 |
$118.00 |
$682.00 |
50% |
$341.00 |
$0.00 |
$341.00 |
| TOTAL |
$2,250.00 |
$757.00 |
$1,493.00 |
|
$725.90 |
$100.00 |
$767.10 |
*Including $100 deductible as outlined in your policy.
**Billed amounts are based on actual claims and will vary by dentist.
*** The In-Network Allowed amount is based on the Maximum Care PPO CI-5 fee schedule and will vary by area.
Can I see an out-of-network dentist?
Yes.
The Out-of-Network Allowed amount is based on the 80th percentile of Fair Health Data or the office submitted fee, whichever is less.
You are responsible for the applicable amount of coinsurance the policy does not cover based on the OON amount above, plus 100% of the difference between the Out-of-Network Allowed amount and the amount billed by the Out-of-Network provider.
Out-of-Network
Joanne has had her policy for 13 months and has selected an out-of-network dentist for her dental work. She paid $1,350.00 (including $100 deductible) for her dental treatment. Her plan also has a $1000 annual maximum benefit.
| Service |
Billed** |
Allowed*** |
Paid % |
Plan Pays |
Deductible |
Patient Pays* |
| Filling |
$250.00 |
$62.50 |
80% |
$50.00 |
$0.00 |
$200.00 |
| Crown* |
$1,200.00 |
$1,150.00 |
50% |
$525.00 |
$100.00 |
$675.00 |
| Root Canal |
$800.00 |
$650.00 |
50% |
$325.00 |
$0.00 |
$475.00 |
| TOTAL |
$2,250.00 |
$1,862.50 |
|
$900.00 |
$100.00 |
$1,350.00 |
*Including $100 deductible as outlined in your policy.
**Billed amounts are based on actual claims and will vary by dentist.
*** The Out-of-Network Allowed amount is based on the 80th percentile of Fair Health Data or the office submitted fee, whichever is less.
 Live Chat
Live Chat